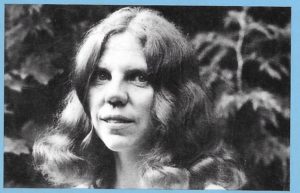
CIRCUMCISION- THE PAINFUL DILEMMA, by Rosemary Romberg, 1st Edition
Chapter Eleven: Complications of Circumcision (Condensed)
Bergin & Garvey Publishers, Massachusetts, 1985
All medical procedures, especially those involving surgery, can and do result in complications. Circumcision is certainly no exception.
Parents rarely know even the simplest details about infant circumcision; much less often do they have any awareness that the operation can have complications. Even doctors are frequently unaware of the many complications that can result from circumcision. Commonly doctors pronounce infant circumcision a “simple operation with few risks.” However, the risks are many and can be devastating and tragic.
It is difficult to accurately document the precise rates of circumcision complications because some difficulties are either never reported or are never attributed to circumcision…
When viewed in terms of individuals and families involved in these tragic events –particularly when the operation is unnecessary — the risks are quite significant.
Upon reviewing the literature, nearly all from medical publications, I have discovered 28 different complications that can result from circumcision. Some of these interrelate or cause other complications. They are listed here in approximate order of frequency:
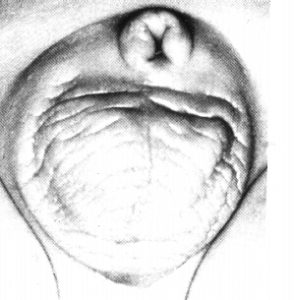
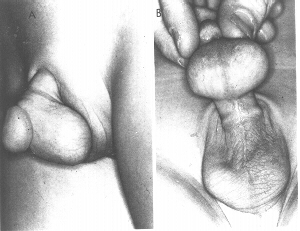
Meatal Ulceration
Many infants and toddlers in diapers develop “urine burns” from contact with ammonia in urine-soaked diapers. … The destruction of the foreskin creates an abnormal state in which the glans is exposed and in constant contact with outer clothing, and for the infant, with urine soaked diapers. Ammonia burns on the glans, especially around the urinary opening, which is known as the meatus, can be a particularly troublesome problem for the circumcised male infant.
40
Meatal Ulceration. (Photograph contributed by John C. Glaspey, M.D.)
41
Meatal Ulceration. (Photograph contributed by John C. Glaspey, MD.)
The incidence of meatal ulceration among circumcised infants is very common… The true incidence of meatal ulceration is undoubtedly much higher than reported. Many cases are undoubtedly treated by the parents with over-the-counter ointments and are never brought to the doctor’s attention.
Ironically, parents upon contemplating circumcision are frequently warned about the supposed “problems” that the child will have if he keeps his foreskin and are given the erroneous advice that the penis of the circumcised child requires no care. Many doctors who regularly treat the sore, eroded, and encrusted glans of the circumcised child apparently lack awareness that the protective foreskin would have prevented this.
The foreskin of the intact infant can occasionally become reddened and swollen. Some doctors believe that this is an indication for immediate circumcision. … In actuality the swollen, red foreskin is performing its function of protecting the sensitive glans from more painful and troublesome irritation.
42
Meatitis in an 11 -month old child. (Kaplan)
Mild topical ointments are usually recommended for meatal ulceration and other urine burns. Petroleum jelly, or petroleum-based germ killing substances containing antibiotics are often prescribed..
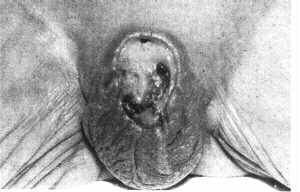
Meatal Stricture
Meatal stricture results from prolonged or repeated episodes of meatal ulceration. The repeatedly irritated meatus becomes narrowed. This results in pain and difficulty with urination. In extreme cases this can result in infections and kidney problems.
One doctor claims that different types of circumcision devices result in varying degrees of “pinpoint meatus,” stating that the Plasti-bell results in more incidence of narrowed meatus. 10.
Berry and Cross calibrated the urethral meatuses of 100 circumcised and 100 intact adult males, and did a similar study of 100 each of intact and circumcised infants. In both groups the urethral meatuses were significantly narrower among the circumcised individuals than among the intact individuals. Men undergoing circumcision early in life showed a higher incidence of meatal narrowing than did those circumcised later.
The results among infants were not as marked, indicating that narrowing of the meatus develops over time. 11.
43
Meatal stenosis from recurrent meatitis in a 13-month old child. (Kaplan)
The most common treatment for the condition is “meatotomy”-a snipping of the urinary meatus to enlarge the opening.
Hemorrhage
Hemorrhage is defined as excessive bleeding. It can result from any event that ruptures blood vessels, including any cut or surgical procedure. Hemorrhage is a fairly common complication of circumcision.
Shulman etal list it as the most common (immediate) complication. They state that bleeding may be caused by inadequate hemostasis (compressing of blood vessels), by abnormalities of blood coagulation, or by anomalous vessels. 14.
Treatments include application of adrenaline-soaked gauze sponge to the bleeding site, ligature (tying off) of a blood vessel, Gelfoam (chemical foam to stop bleeding), silver nitrate stick, or topically applied thrombin, retying of Plasti-bell string, and administration of cryoprecipitate. 15.
Occasionally babies have required blood transfusions as a result of post-circumcision hemorrhage. One doctor tells of his experience:
I spent a considerable portion of one evening transfusing an infant circumcised by an expert Rabbi. The hemorrhage had to be controlled in the operating-room and the baby was hospitalized for two days…. I know of other cases needing transfusion under the same conditions and I have seen several babies considerably anemic owing to the insidious loss of blood which is easily overlooked for several hours. 16.
Babies have died from post-circumcision hemorrhage. Since Biblical times the Jews have had a law that if two sons of the same mother bled to death following circumcision, any future sons were exempt from the ritual. This indicates that hemorrhage has always been a complication of circumcision. …
Finally, undetected hemophilia can produce drastic results if such an infant is circumcised. Occasionally hemophilia is discovered when the infant undergoes circumcision and subsequently hemorrhages.
Infection
Infection of the fresh circumcision wound has been a fairly common complication. I have found more reports of this incidence than of any other complication. Infection has occasionally been accompanied with disastrous results, including death. Some of the other complications described elsewhere in this chapter, such as loss of penile skin, have resulted from infection of the circumcision wound.
Any open area of skin is a potential avenue for infection. Because the freshly circumcised infant penis is in constant contact with wet and/or soiled diapers, this area cannot be kept sterile. …
Particularly antibiotic-resistant strains of bacteria and other infectious agents abound in hospitals. Newborn infants are not as able to resist infection as are older individuals who have built up more immunities. It is not uncommon for newborns in busy hospital nurseries to develop infections, particularly Staphylococcus-based. Sometimes babies do not manifest symptoms of infections until they are home from the hospital.
A 1960s study … cited the umbilical stump and the freshly circumcised penis as the major sites of highest concentrations of Staphylococcus aureus to be found, saying “the blood on the cord and the circumcised penis provide an excellent media for growing bacteria.” 20.
A wide variety of different infections with the circumcision site as port of entry have been listed by different sources. Besides Staphylococcus aureus, other infections include Staphylococcus epidemidis, Klebsiella pneumoniae, Escherichia coli, and Proteus mirabilis. 15.
Scurlock and Pemberton report four cases of “fulminating neonatal sepsis with meningitis.” In other words, infection of the circumcision site resulted in infection of the spinal cord and brain. 21.
In another report Annunziato and Goldblum describe severe staphylococcus infections originating from the circumcision site which they call “scalded skin syndrome.” They describe three cases of infants with skin red and peeling, pustules, circumcised area red, swollen, and covered with profuse thick, yellow-green exudate. The infants were feverish, lethargic, cyanotic, and had diarrhea. After administration of antibiotics, two infants healed normally and one died. 22.
Sussman, Schiller, and Shashikumar describe a type of infection which they call “Fournier’s Syndrome.” They describe three cases of this condition, one resulting from a burn, and two from infected neonatal circumcision. Their descriptions include extensive gangrenous ulcerations around the base of the scrotum, tip of the penis, and in the perineum, with the skin sloughing off. The infants healed following treatment with antibiotics, but scarring remained. 23.
Sauer reports a fatal staph infection following ritual circumcision. On the 13th day the infant exhibited fever, pallor, and lack of appetite. The circumcision blade had cut away a slight amount of the glans, which appeared to be the center of the infection. Antibiotics were given. On the 18th day of life several cc. of blood and mucus were vomited spontaneously and the infant expired before medical aid arrived. Autopsy revealed 6ver 50 gray abscesses in the lungs. The infecting agent was Staph Aureus. The circumcision wound was nearly healed at the time of death. 24.
Kirkpatrick and Eitzman describe two cases involving premature infants who developed infections after being circumcised with the Plasti-bell device.
Routine circumcision is often recommended because of the possibility of “infection.” In truth any part of the body can become infected. Intact men and boys can develop infections of the foreskin. This type of infection is invariably mild and local in nature. It usually can be remedied easily with proper washing, without resort to any drastic measures. This minor type of infection does not begin to compare with the potentially disastrous consequences of an infection of a fresh circumcision wound. It appears that authorities have been concerned about the wrong kind of infection.
Retention of Plastic Bell Ring
If a Plasti-bell device is used to circumcise a baby, the remaining foreskin should dry up and fall off with the ring within about 10 days after the operation. A complication peculiar to this device occurs when the ring fails to fall off and instead becomes buried under the skin along the shaft of the penis.
Concealed Penis
An unusual complication occurs when the penile shaft, following circumcision, retreats into the surrounding skin and fatty area and cannot be seen. This problem must be corrected by surgery, and often skin grafting, to produce a normal penis.
Drs. Shulman, et al., describe this occurrence:
The penis is forced into a subcutaneous position by wound contraction following circumcision. This may be produced if there is a tendency of the penis to retract into the fatty mons pubis, and later the circular wound heals, contracts and holds the penis in a submerged position beneath the pubic skin. 30
??
Left, Concealed penis prior to operative exposure.
Right, Penis after exposure of glans and suture of inner surface prepuce to skin. (Trier)
Left, Concealed penis. Bulge of glans is seen under skin.
Right, Glans exposed and held by traction suture. Suture line of inner surface prepuce and penile skin is visible. (Trier)
Concealed penis after circumcision (Kaplan)

Repair of concealed penis. The inner preputial epithelium has been folded back to provide skin cover. (Kaplan)
Urethral Fistula
A fistula is an abnormal opening in any part of the body. A urethral fistula is a hole going from the side of the male urethra to the outside of the penis. Usually the fistula occurs on the underside. This can develop as a result of circumcision. It results either from accidental crushing of the urethra by the circumcision clamp, an abnormality in the urethra, or from a stitch placed in the underside of the penis to control excessive bleeding at the site of the frenulum.
47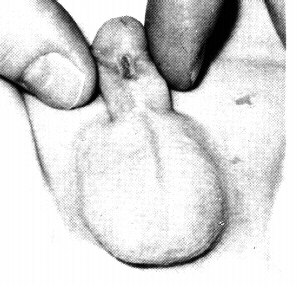
Urethrocutaneous fistula following circumcision.(Kaplan)
Phimosis of Remaining Foreskin
Phimosis refers to any condition in which the foreskin cannot be retracted. This condition is normal in the intact infant, and is not true phimosis. Occasionally the older intact male may have a tight foreskin that is difficult to retract. This condition can usually be resolved by simple methods, and does not need to be corrected by circumcision. One of the purported arguments in favor of routine neonatal circumcision is that the operation will supposedly prevent phimosis. This is proven untrue, for occasionally the remaining piece of foreskin becomes tightly attached to the sides of the glans and the infant then must undergo a painful loosening procedure or possibly a second circumcision.
Urinary Retention
Occasionally a baby will not urinate for several hours following circumcision. Sometimes the cause is an overly tight bandage wrapped around the wound. In other instances the cause is less clear.
It is conceivable that similar urinary retention could result from an overly tight plastic bell ring. There have also been instances of infants failing to void for several hours following circumcision when no bandage or plastic ring was in place. This may be a psychological response on the infant’s part to the trauma of the operation.
Glans Necrosis
Necrosis refers to the death of body tissue. This has happened to the glans following circumcision due to an overly tight bandage or a Plasti-bell ring that is too small.
Kaplan describes this occurrence:
On occasion, in an attempt at hemostasis, the circulation to the glans penis may be compromised, resulting in either cyanosis or necrosis of the glans penis. I was asked to see a child with cyanosis of the glans penis one day following circumcision. Many sutures were present. Additionally, an anaerobic streptococcus was cultured from the wound so that it was not clear whether the cyanosis was secondary to the sutures used or to an underlying infection. With removal of the sutures and use of antibiotics, this problem resolved without tissue loss. 43.
Injury and Loss of Glans
Occasionally the glans can be injured or entirely cut off during circumcision. Usually a permanent deformity results. Both the Plasti-bell and the Gomco clamp employ the protective “bell” which covers the glans before the clamp or string is applied, thus precluding injury to the glans. Other methods not employing a “bell” pose greater risk of injuring the glans. The glans can also be injured before the bell is in place, during the dorsal slit procedure, or as the operator frees the foreskin from the glans.
Excessive Skin Loss
A newborn baby’s penis is very tiny. Usually only about one-half inch of skin is amputated during circumcision. Some operators tend to take off more than others, consequently there are many “varieties” of circumcised penises. Some males have no remaining foreskin while others have a sizeable ring of skin left in place.
Considerable debate abounds over what is the “right” amount of foreskin to cut off. (Hopefully soon we will decide that the best answer is “none!”) Taking off a small amount of skin can result in phimosis of the remaining foreskin with possible need for repeat circumcision. However, devastating complications result from cutting off too much skin. The fact that the ultimate size of the penile shaft, proportionate to the foreskin, is not attained until later in life, further complicates the matter. A newborn’s foreskin usually extends far beyond the glans. It may appear overly long, but as he matures he will in effect “grow into it.”
Excessive skin loss can result from the operator severing too much foreskin, from infection of the wound resulting in tissue death, or from a burn caused by an electrocautery device. Sometimes the entire penile shaft becomes denuded and skin grafting is necessary. Other times the results are less drastic and the wound heals, but as the individual grows older his penile skin becomes too tight, causing discomfort on erection.
Skin Bridge
“Skin bridge” can result from circumcision. It is a complication in healing of the wound, by which a piece of skin from the shaft of the penis has become attached to the glans, or another point along the shaft, forming a “bridge” that must be surgically corrected.
48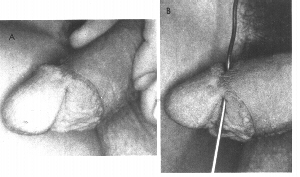
Left, patient with a skin bridge. Right, a probe has been passed under the bridge (Kaplan)
Vomiting, Apneic Spells
Apnea (British spelling apnoea) means cessation of breathing, usually for a short period of time. Sometimes normal healthy infants have spells of apnea during sleep and it is of no consequence. However, sometimes this event can be life-threatening.
Fleiss and Douglass report:
A healthy 1-week-old infant had a circumcision done by a well-trained and experienced physician without any anaesthetic. The infant tolerated the procedure well except for excessive crying, which began at the time of the operation. The mother, attempting to soothe her distressed infant, resumed breast feeding after the operation. An episode of vomiting followed the feeding. An apnoeic spell followed the emesis. The infant was taken to a local emergency room and subsequently transferred to [a children’s hospital]. He received a complete septic workup, intravenous antibiotics and hospitalization for five days of observation until the cultures were negative and sepsis was ruled out. The infant was discharged from the hospital six days after circumcision doing very well.
Infants do feel the pain of the surgical removal of the foreskin performed without any anaesthetic, and they respond to the pain by crying. That crying may be excessive. Air may be swallowed. Mothers do soothe their infants by feeding them. Vomiting may follow the feeding. Apnoea may follow vomiting .. 51.
Sewing of Penile Skin to the Glans
Stitches are not normally required following neonatal circumcision, so presumably this bizarre complication has resulted from circumcision performed on older individuals.
Browne mentions:
Sewing the skin edge to the glans, with consequent burying of the corona. This mistake arises from not retracting the mucosa fully. It entails a tedious little dissection. 37.
Laceration of Penile or Scrotal Skin
Circumcision jokes often center around, “What if the knife slips?” This feared event has happened. Shulman etal report:
Accidental laceration of the penile skin and scrotum following circumcision has been seen in 2 cases…. [In one case] the Mohel slipped during the performance of the operation, and the knife opened the ventral surface of the penis and scrotum and exposed both testes. The skin was sutured under general anesthesia six hours after the accident and healing was uneventful. 52.
Undetected Hypospadias
Hypospadias is a congenital deformity in which a fistula naturally occurs in the underside of the penis. This is corrected by plastic surgery. The foreskin provides an easily available piece of tissue for use in skin grafting. (Thereafter, the individual is essentially circumcised, but at least the foreskin has provided a correction for the defect.) If an infant with hypospadias is routinely circumcised, this potentially useful piece of skin has been destroyed and the operator must resort to more complicated types of skin grafts to reconstruct the penis.
Preputial Cysts
A cyst is an abnormal, closed pocket of body tissue which contains fluid or solid material. Occasionally cysts develop along the remaining edge of foreskin at the site where the skin was severed.
Kaplan discusses this:
These occur either by rolling in epidermis at the time of circumcision, or perhaps by implanting smegma in the circumcision wound. These inclusion cysts may grow to rather large proportions…. Even those that remain small can become infected…. Obviously the treatment is surgical excision. 53.
Preputial inclusion cyst following circumcision.
A. lateral view. B. ventral view of the same patient.(Kaplan)
Complications of Anesthesia
Complications can ensue from use of any type of anesthesia for any medical procedure, including circumcision.
Critics of infant circumcision frequently express outrage that newborn infants are usually given no anesthesia for an operation considered painful enough to warrant anesthesia for an older child or an adult. However, administration of such drugs to newborn infants is riskier than anesthetizing an older individual. Certainly if all newborn infants undergoing circumcision were being given general anesthesia for the operation we would see many more cases of death or difficulty from the anesthetic.
Tuberculosis and other Diseases from Mezizah
Mezizah is the third step of the Jewish ritual circumcision ceremony, in which the mohel applies his mouth to the fresh circumcision wound. Diseases have been spread due to this practice. Today, few ritual circumcisors practice it.
According to Bromley:
A few years ago [19291 one of our leading medical journals published an account of an infected operator, who, during the third stage of the operation [mezizah] had infected seven children with tuberculosis and it proved fatal to all within a short time after this religious rite. 54.
Strangulation of the Glans by Hair
Medical reports have described cases of small boys who have, either accidentally or intentionally, had long strands of human hair tightly wrapped around the coronal sulcus (the indentation beyond the outer rim of the glans). This can be considered an indirect complication of circumcision, because the intact penis with the foreskin covering the glans has one smooth continuous surface and the glans and the coronal sulcus are not exposed.
Recurrence of Pneumothorax
A pneumothorax is a collection of air or gas in the membranes that surround the lungs or pleural cavity. Auerbach & Scanlon tell of a case involving an infant who developed a. pneumothorax as a result of mechanical assistance with breathing for severe respiratory distress at birth. After it was treated the infant was circumcised. His excessive crying from the pain of the operation caused the pneumothorax to recur:
Pulmonary Embolism
A pulmonary embolism is a clot of blood which travels through the circulatory system and becomes lodged in one of the blood vessels in the lungs. This causes severe breathing difficulties and can result in death. This is a small but potential risk of any surgery.
Keloid Formation:
A keloid is an abnormal development consisting of a raised, firm, thickened, red piece of scar tissue. Such a formation at the site of circumcision creates a grotesque deformation of the organ, with obstruction of its function.
Ecstein describes an extensive keloid scar which developed on a small boy 6 months after he was circumcised “without any good clinical indication.” 58
Lymphedema or Elephantiasis of Skin
These terms refer to the swelling or obstruction of the lymph vessels. This can result from circumcision. According to Shulman, et al.:
A baby with lymphedema of the penis had been circumcised at 8 days. He was referred at age 10 months. Several days after circumcision the penis and scrotum had become swollen. On examination at 25 days it was found that a large portion of the prepuce remained and covered the glans. The penis and scrotum were edematous. Several weeks later the scrotal edema regressed but the penile skin of the ventral surface remained edematous. On admission, marked edema of the lower part of the penile skin was found…. At operation, the lymphedematous tissue was excised down to the penile fascia. The defect on the ventral surface was easily closed by the remaining dorsal flaps. 30.
50
Distal lymphadema following circumcision complicated by wound separation and infection.(Kaplan)
Reaction of Older Sibling
Perhaps the following experience can be considered a complication of circumcision. A doctor reports:
One Sunday afternoon I received an urgent call from a harassed mother who informed me that her two-year-old son had tried to amputate his penis and was bleeding profusely.
He had a moderately deep laceration half-way around the base of the penis. The urethra was intact. The laceration was sutured and recovery was uneventful.
The youngster had witnessed his baby brother’s ritual circumcision one week previously and had obviously been impressed by the procedure and all the attention his brother had received. 59.
Cosmetic Problems
The Gomco clamp and Plasti-bell devices produce an even circular cut … Older methods such as smashing the skin with a hemostat and slicing it off present greater risk that an uneven cut will result. Browne uses the quaintly British expression: “Untidy tags of skin.” 37
Removal of only a tiny bit of foreskin can cause dissatisfaction on the part of parents who are conditioned to believe that the denuded state is preferable. Sometimes such parents will take their babies back to the doctor to have more foreskin cut off because they believe that his penis does not look circumcised enough.
Loss of Penis:
I have purposely saved the most dramatic and devastating complication for last. There have been cases in which the penis has been lost due to circumcision, caused by mishandling of the operation, as a result of an infection, or by a burn from electrocautery technique. In some cases enough penile shaft remained so that after extensive operations a functional penis could be reconstructed. In other cases the child has been surgically made into a girl.
Hamm and Kanthak describe two infants who underwent penile reconstruction:
Two cases of gangrene of the penis in newborn infants occurred following circumcision for which a high frequency cutting current was utilized. In each instance the procedure was done by the physician in this way for the first time and had been utilized in the hope that a simple, hemostatic method of circumcision would result. Each of these cases was attended by more or less complete sloughing of the external portion of the penis resulting, on spontaneous healing, in a flat, smooth area of skin continuous with the scrotum on which no evidence of penile projection was present. In each of these cases a satisfactory penis was reconstructed.
… The penis has been reconstructed utilizing the remains of the corpora cavernosa penis and the corpus cavernosum urethrae with its enclosed urethra….
Repair of the penis utilizing the remains of the penile stump by exteriorizing the deep portions of the corpora cavernosa and covering the newly formed shaft with a free skin graft provides a direct approach and a penis composed of more physiologically normal elements than is otherwise possible. 61.
Total penile slough due to electrical burn of penis during circumcision. (Kaplan)
There are documented cases of sex-change due to total loss of the penis following circumcision.
Being female is wonderful if one is born that way. But one can only begin to speculate the anxieties and identity problems that an unwittingly converted female will experience as she grows up.
Photographs:
Photograph contributed by John C. Glaspey, M.D.
Kaplan, George W., “Circumcision — An Overview,” Current Problems in Pediatrics, Vol. 7, No. 5, March 1977
Trier, William C., M.D., & Drach, George W., M.D., “Concealed Penis,” American Journal of Diseases of Children, Vol. 125, Feb. 1973
Selected References:
10. Graves, John, M.D. “Pinpoint Meatus: Iatrogenic?” Pediatrics, Vol. 41, 1968, p. 1013.
11. Berry, Carl D., Jr., M.D. and Cross, Roland R., Jr., M.D. “Urethral Meatal Caliber in Circumcised and Uncircumcised Males” A.M.A. Journal of Diseases of Children, Vol. 107, Feb. 1961, p. 149.
14. Shulman, J., M.D.; Ben-Hur, N., M.D.; and Neuman, Z., M.D. (Israel) “Surgical Complications of Circumcision” American Journal of Diseases of Children, Vol. 107, Feb. 1961, p. 149.
15. Gee, William F., M.D., and Ansell, Julian S., M.D. “Neonatal Circumcision: A Ten-Year Overview” Pediatrics, Vol. 58, 1976, p. 827.
16. Banister, P.G. “Circumcision” The Lancet
20. Kravitz, Harvey, M.D.; Murphy, John B., M.D.; Edadi, Kasem, M.D.; Rosetti, August, M.D.; & Ashraf, Hebatollah, M.D. “Effects of Hexachlorophene-Detergent Baths in a Newborn Nursery with Emphasis on the Care of Circumcisions” The Illinois Medical Journal, Vol. 122, No. 2, August 1962, p. 133-139.
21. Scurlock, Jacqueline M., M.B., B.S., & Pemberton, Patrick J., M.B. “Neonatal Meningitis and Circumcision” The Medical Journal of Australia, March 5, 1977, p. 332-333.
22. Annunziato, David, M.D., & Goldblum, Louis M., D.O. “Staphylococcal Scalded Skin Syndrome – A Complication of Circumcision” American Journal of Diseases of Children, Vol. 132, Dec. 1978, p. 1187-1188.
23. Sussman, Sidney J., M.D.; Schiller, Ruth P., M.D.; & Shashikumar, V.L., M.D. “Fournier’s Syndrome” American Journal of Diseases of Children, Vol. 132, Dec. 1978, p. 1189-1191.
24. Sauer, Louis W., M.D. “Fatal Staphylococcus Bronchopneumonia Following Ritual Circumcision” American Journal of Obstetrics, Vol. 1, No. 46, 1943, p. 583.
30. Shulman et al., p. 152.
43. Kaplan, George W., “Circumcision — An Overview,” Current Problems in Pediatrics, Vol. 7, No. 5, March 1977, , p. 28.
51. Fleiss, Paul M., & Douglass, John “The Case Against Neonatal Circumcision” British Medical Journal, September 1979, p. 554.
52. Shulman, et aL, p. 150.
53. Kaplan, p. 26.
54. Bromley, R. Innis “Circumcision” Medical Journals and Records, August 21, 1929, p. 212-213.
58. Ecstein, Herbert B. “Minor Surgery in Infancy and Childhood” Update, January 15, 1979, p. 141, 144.
59. Lewin, Peter, M.D. “Ritual Circumcision Sequel” Clinical Pediatrics, October 1971, p. 583.
61. Hamm, William G., M.D., & Kanthak, Frank F., M.D. “Gangrene of the Penis Following Circumcision With High Frequency Current” Southern Medical Journal, Vol. 42, No. 8, Aug. 1949, p. 657-659.